An Essential Guide to AI Healthcare Technology for Practices
In the modern healthcare landscape, merely using digital patient engagement tools is no longer enough to provide the best possible patient journey; your success in using these tools depends on how intelligently you use them. Enter artificial intelligence (AI) tools.
AI is more advanced and accessible than ever before, and adopting it is the only way for care teams to keep up with evolving clinical and administrative needs. With studies showing that the US patient engagement market is projected to grow from $29.33 billion in 2025 to over $51 billion by 2030, there’s never been a better time to use AI tools. That’s where this guide comes in!
Let’s explore the current state of AI in healthcare, addressing the operational, ethical, and financial realities that decision-makers face going forward.
Table of Contents:
- AI healthcare technology FAQs
- 15 top AI healthcare technology use cases
- How to implement AI healthcare technology
- Other essential best practices for using AI patient engagement tools
- What's the best AI healthcare technology?
AI healthcare technology FAQs
What is AI in healthcare?
Before diving into healthcare use cases, we should define three related but distinct terms:
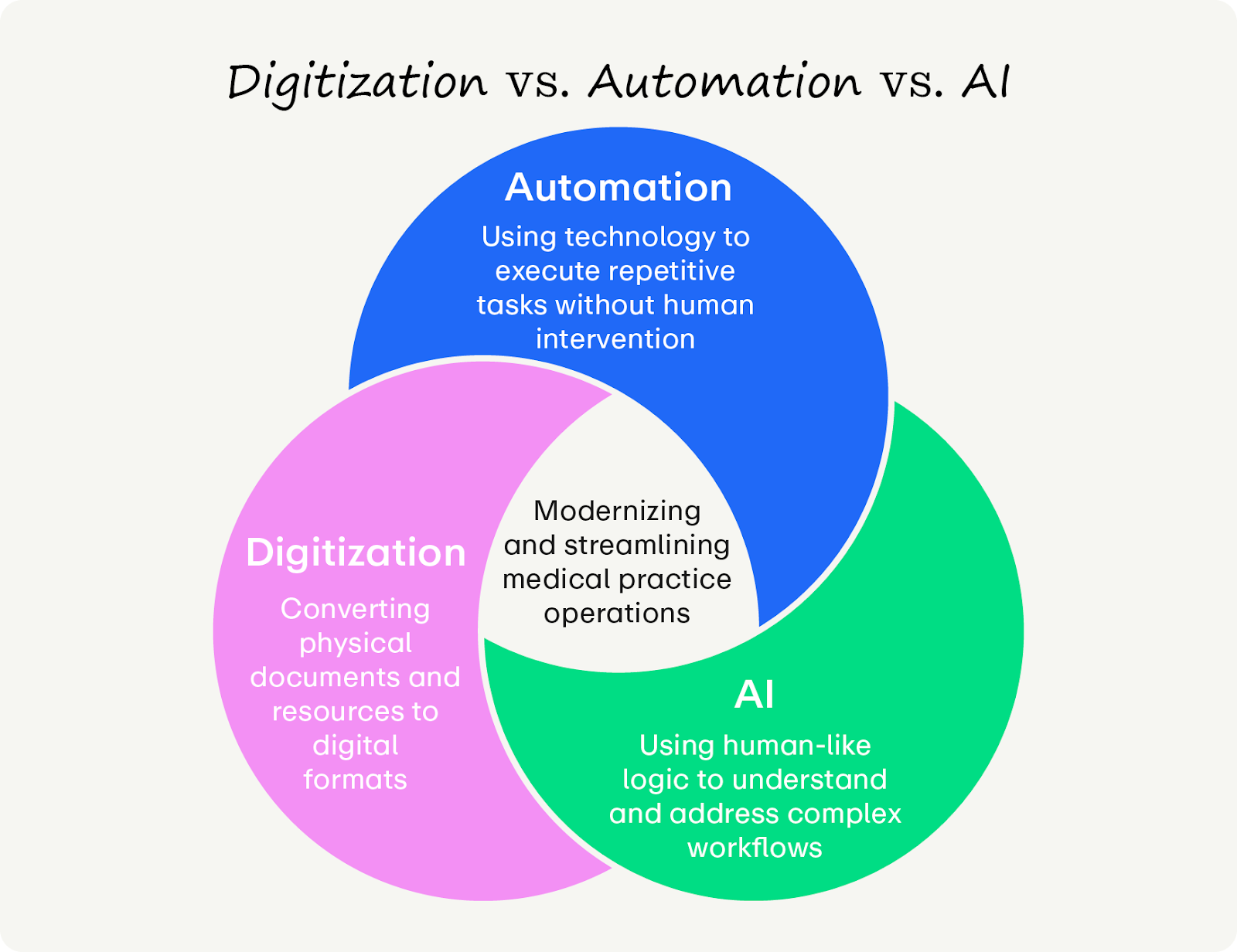
- Digitization is the process of converting information from an analog to a digital format. In a medical context, this typically involves scanning paper documents (like patient information) into static PDFs. Digitization still requires humans to run the process.
- Automation is the application of technology to execute repetitive, rule-based tasks without human intervention. Unlike digitization, automation utilizes technology to actively extract structured data from digital forms and populate the corresponding fields in your practice management (PM) system, effectively eliminating the labor of manual data entry.
- AI is technology that can complete complex tasks using human-like logic and reasoning. AI is present throughout many aspects of healthcare management, from scheduling patients to facilitating payments (we’ll discuss more use cases later).
Most practices use a combination of these technologies, depending on their chosen software. We’ll review ideal use cases later.
What are the benefits of using AI patient engagement strategies?
AI’s impact goes beyond saving time. Used well, AI-powered workflows can future-proof your practice by enabling:
- 24/7 operational access. AI chatbots and virtual assistants provide patients with round-the-clock support, answering queries and scheduling appointments even when the office is closed. This ensures patients receive timely service regardless of staffing hours, boosting their satisfaction.
- Hyper-personalized care. Unlike generic patient portals, AI analyzes individual medical history and behavior to tailor communication. For example, you might use AI to send specific health tips or medication reminders that resonate with a patient's unique needs. This level of customization fosters deeper engagement and empowers patients to take an active role in their health.
- Proactive risk mitigation. Predictive analytics enable systems to identify high-risk patients before issues escalate, such as predicting the likelihood of readmission or flagging non-adherence to treatment plans. This additional perspective helps your staff provide the highest quality of care and prevent issues before they happen.
- Revenue protection and efficiency. By automating routine tasks such as billing and appointment reminders, AI reduces administrative waste and minimizes costly no-shows. Some providers have reported a 34% reduction in missed appointments using AI-driven identification of high-risk no-show patients.
Is AI healthcare technology HIPAA compliant?
AI handles large quantities of sensitive patient data, so it’s essential that your tool follows the strictest standards for HIPAA compliance.
Modern AI platforms use SOC2 Type 2 security protocols and zero-retention data processing. This ensures that while the AI analyzes data to generate a schedule or a clinical note, the data is not used to train public Large Language Models (LLMs) and is encrypted from end to end. Additionally, conducting security audits and having tiered access controls for users are best practice to ensure sensitive patient information never leaves secure databases.
How should clinical or administrative staff interact with AI?
A common concern with AI in healthcare is its potential impact on the workforce and the roles of care providers. It's important to understand that AI healthcare technology is designed to augment your team's capabilities, not replace them. AI acts as a force multiplier, alleviating the majority of repetitive, low-value tasks that often contribute to clinician burnout.
This allows the human staff to focus on the work that requires emotional intelligence and medical skill instead of more menial tasks. In most cases, AI acts as an initial line of defense, flagging potential risks for a human to review rather than acting autonomously.
15 top AI healthcare technology use cases
Administrative and scheduling efficiency
- Predictive no-show prevention: Beyond simple reminders, AI can score every appointment based on the likelihood of a no-show—if the risk is significant, it can send remind the patient of the appointment to mitigate no-shows.
- Round-the-clock intelligent scheduling: AI agents can book, reschedule, or cancel appointments via text or web 24 hours a day, capturing traffic that occurs outside of business hours.
- Real-time insurance verification: AI agents verify insurance eligibility, remaining deductibles, and co-pays at the moment of booking, reducing the administrative burden on the front desk and the risk of surprise bills for patients.
- Automated waitlist management: When a cancellation occurs, the AI instantly polls the waitlist for the best-fit patient and reaches out to them in seconds to maximize appointments and revenue.
- Patient reactivation sequences: AI identifies patients who are overdue for a follow-up or preventative screening and initiates a conversation to get them back on schedule.
Clinical support and patient monitoring
- Hardware-free vital capture: Using high-definition cameras and imaging, AI can now offer a ballpark measurement of heart rate, blood pressure, and oxygen saturation without requiring a physical cuff or wearable (but humans should still check the tool’s work!).
- Ambient clinical documentation: AI scribes listen to the patient-doctor encounter and generate a structured SOAP note in real-time, saving clinicians hours of charting daily.
- Symptom-based triage: Digital intake forms can use AI to adapt their questions based on patient input, ensuring high-acuity patients are flagged for immediate review while low-acuity cases are routed to less urgent channels.
- Post-discharge safety nets: Automated check-ins can identify areas of concern in a patient’s recovery based on their follow-up notes, alerting the nursing team only when an intervention is necessary.
- Multilingual patient education: AI can instantly translate discharge summaries and medication instructions into the patient's native language while ensuring medical terminology remains accurate.
- Remote Patient Monitoring (RPM) synthesis: Instead of flooding providers with raw data from wearables, AI synthesizes large quantities of patient vital data into a single “stability score.”
Financial and revenue cycle management
- Automated financial counseling: AI calculates a patient’s out-of-pocket responsibility in real-time and offers personalized payment plans or "text-to-pay" links immediately after the visit.
- AI-driven coding optimization: AI analyzes the clinical note against the latest ICD-10 and CPT guidelines to ensure the most accurate code is suggested, minimizing claim denials.
- Propensity-to-pay analytics: AI-powered tools identify patients who may struggle with high balances and proactively offering financial assistance options before the bill goes to collections.
- Denial management automation: AI agents can read an EOB (Explanation of Benefits), identify why a claim was denied, and draft the corrected claim or appeal letter automatically.
How to implement AI healthcare technology

1. Standardize AI policies
A lack of standardization is the biggest barrier to productive, safe AI use. Shadow AI is the unauthorized use of consumer-grade generative AI by staff members to complete clinical or administrative tasks. For example, a physician might use a public chatbot to summarize a patient’s history, or a receptionist might use it to draft a sensitive email.
Because these public tools are not HIPAA-compliant and lack clinical validation, they pose a massive liability. To manage these risks, practices must create an AI usage policy. Health practice use policies should include:
- Permitted and prohibited use cases that clearly define which AI tools and applications are allowed for staff and in what capacity, and which are strictly forbidden.
- Data handling and privacy that mandates that Protected Health Information (PHI) and confidential patient data must never be entered into non-HIPAA-compliant AI systems.
- Clinical review requirement that stipulates that any AI-generated clinical content (e.g., diagnoses, treatment plans, medical summaries) must be thoroughly reviewed and validated by a licensed clinician before use or inclusion in the patient record.
- Transparency and disclosure requirements that require staff to inform patients when AI has been used in their care when they ask (e.g., an AI-generated draft note).
- Training and education that outlines mandatory training for all staff on the policy, risks, and responsible use of AI in a healthcare setting.
- Accountability and enforcement policies that detail the consequences for violations.
Every practice will have unique practice requirements, but your use policy should contain this information as the foundation.
2. Identify high-friction bottlenecks
The first step in a successful AI rollout is identifying where your practice is losing revenue or staff time. Work with your staff to conduct a friction audit that answers these questions:\
- Where do patients experience the most frustration in their journey with your practice?
- Which administrative tasks consume the most staff time?
- What is your current no-show rate, and at what stage in the scheduling process are those appointments typically missed?
- What percentage of patient calls are abandoned or result in a long wait time?
- What are the most common reasons patients contact your practice outside of a scheduled appointment?
- What’s your post-visit payment collection rate?
- What’s your patient retention rate?
By starting with a specific problem, you can choose an AI tool that delivers an immediate, measurable win, which is essential for earning stakeholder buy-in.
3. Ensure bidirectional system integrations
The best AI tools don’t operate in a vacuum. Bidirectional integration with your PM systems ensures that when a patient updates their medical history or schedules a visit via AI, that information is automatically updated in the master record without human intervention.
Pro-tip: To avoid integration headaches, look for a patient engagement platform with PM management tools that’s powered by AI so you can run your practice from one convenient location (more on that later).
4. Establish a governance policy with human oversight
To maintain clinical safety and trust, you must implement a human-in-the-loop framework. This means that while the AI performs the heavy lifting, a qualified human must always review and validate the output before it becomes part of the permanent record. This policy protects the practice from AI errors and ensures that the final clinical decision comes from the medical professional.
5. Launch a pilot phase
Taking on a full AI rollout can overwhelm your staff and actually present more bottlenecks than fixes. Instead, select a single location or a provider to pilot the technology for 30 to 60 days. Monitor key performance indicators (KPIs) such as interaction abandonment rates, staff hours saved, and patient satisfaction scores. Use this pilot data to pivot your settings and use policies before scaling the solution to the rest of the organization.
Other essential best practices for using AI patient engagement tools

1. Establish an AI governance committee
AI oversight can no longer be an IT-specific task. Practices should assemble a multidisciplinary AI Governance Committee that includes clinical leads, administrative managers, and compliance officers. This group is responsible for maintaining an AI Inventory, which is a comprehensive list of alby catel tools currently in use, their specific functions, and their data dependencies. By centralizing oversight, you prevent Shadow AI and ensure that every new tool aligns with the practice’s overarching strategic and ethical goals.
2. Understand each tool’s power
AI tools operate differently and have unique features. A best practice for modern administrators is to classify tools on a three-level autonomy scale with these levels:
- Level 1: Limited Autonomy
- Use case: AI-powered transcription services that convert doctor-patient conversations into text, requiring a human clinician to review and finalize the documentation.
- Level 2: Semi-Autonomous
- Use case: Diagnostic support tools that analyze medical images to flag potential abnormalities, but a final diagnosis and treatment plan must be made by a physician.
- Level 3: Agentic Autonomy
- Use case: AI-powered diagnostic imaging system that autonomously analyzes data from multiple sources, flags potential issues, and prioritizes critical cases in the provider’s queue, requiring human review for final confirmation.
By categorizing tools by risk level, you can align the degree of human oversight required. High-risk clinical tools require continuous validation and real-time human intervention, while low-risk administrative tools can be managed via periodic quality audits.
3. Monitor for performance
AI systems’ accuracy can drift as clinical protocols change, patient demographics shift, or vendor updates occur. That’s why you need a schedule for post-deployment monitoring. This involves regularly auditing AI outputs against gold-standard human assessments to identify any decline in reliability. For example, if an AI coder’s accuracy drops after a new software update, the governance team must be equipped to pause the tool and retrain staff or adjust the algorithm.
The frequency of these updates depends on the quantity and type of AI tools you use. For instance, a smaller ophthalmology practice that primarily uses patient engagement software to schedule appointments likely only needs to check in on the software when new updates drop, whereas practices that use AI for agentic procedures should check on it monthly.
4. Conduct bias audits
AI bias is often a reflection of the data it was trained on. To ensure equitable care, practices should demand transparency from vendors regarding their training datasets. A critical best practice is to conduct AI bias audits, which test the tools against your specific patient population. Look for these signs of bias:
- Disparities in diagnosis rates or treatment recommendations across demographic groups
- Inaccurate risk prediction based on socioeconomic factors
- Algorithms that interpret a lack of health data as a sign of good health, rather than a lack of access to care
Ensure your chosen provider has standards for preventing bias in AI datasets and that your AI governance committee is aware of possible bias.
5. Create an anonymous AI feedback channel
learn mo
Encourage staff to report erroneous content, biased risk scoring, or workflow bottlenecks in an anonymous form so they can feel free to express their full opinions. This feedback loop is essential for identifying unintended consequences early and allows the practice to work with vendors on necessary safety patches.
6. Standardize patient disclosure and consent
Trust is the currency of healthcare. Even if not strictly required by law for every minor use case, a best practice is to provide proactive transparency wherever possible. This includes updating your Notice of Privacy Practices to reflect AI usage and providing clinicians with talking points to explain the role of AI in their care. Patients should feel that AI is a tool their doctor uses to provide better care, rather than a tool making decisions without oversight.
What's the best AI healthcare technology?
While many vendors offer specialized solutions for scheduling or billing, the complexity of modern healthcare requires a unified approach. Fragmented tools lead to inefficient workflows and data silos, which ultimately degrade the patient experience.
Promptly stands out as the industry’s premier AI patient experience suite because it was built to solve the entire lifecycle of patient relationship-building within a single, secure ecosystem. Our features and results speak for themselves:
- Intelligent patient access: Our automated waitlist and smart scheduling tools don't just manage appointments; they maximize capacity without staff intervention. Practices using our smart scheduling and communication tools anticipate up to a 90% reduction in no-shows.
- AI-powered intake and efficiency: We use AI and optical character recognition (OCR) technology to automate data entry and insurance verification. Our clients save over 1,700 staff hours annually, freeing teams to focus on patient care.
- Total system consolidation: By replacing fragmented vendors (e.g., intake, payments, engagement, reputation) with one unified AI-powered suite, practices save an average of $88,000 annually and eliminate the data silos that cause operational friction.
Wrapping Up
By consolidating multiple management systems into one intelligent AI-powered platform, Promptly eliminates the costly manual labor and allows your providers to return to what they do best: practicing medicine.
Want to learn more about patient engagement and healthcare technology? Learn more with our resources:
- Master Insurance Eligibility Verification with These Tips. Insurance eligibility verification is essential for ensuring a great patient experience. Improve the process for both your team and patients with these tips.
- An Ultimate Guide to Automation in Healthcare: 15 Use Cases. Learn about other autonomous healthcare technologies in this guide.
- Digital Patient Intake Guide for 2025: Key Insights for Healthcare Practices. Patient intake is usually the first impression patients receive of your practice. Wow them with these tips.
Ready to build future-proof practice operations?
Power up your practice’s workflow with Promptly PaigeAI.
Related Posts
About the author
Dr. Anish Kapur is a physician and tech entrepreneur advancing healthcare through innovation. He co-founded one of the first cloud-based EMR systems for specialists and now leads Promptly Technology Inc., whose Patient Experience Suite™️ helps specialty practices streamline workflows, boost patient engagement, and accelerate revenue—all in one modern platform.

Share this article:






