.png)
Master Insurance Eligibility Verification with These Tips
It happens every day in practices across the country. A patient arrives for their appointment, and during intake, the front desk checks their insurance card, sees the "Active" date, and waves them through. The doctor provides excellent care, the patient leaves happy, and the billing team submits the claim.
Later, the claim bounces back. The reason? "Coverage Terminated" or "Service Not Covered Under Current Plan." By the time you receive this rejection, the patient is long gone. The chances of collecting that full balance from them now are low. You have effectively provided premium medical care for free.
Enter insurance eligibility verification. This essential task ensures your patients receive covered care and your office collects the revenue it needs to keep the lights on. Plus, with the right tools, you can run insurance eligibility verification checks instantly as part of the patient intake process.
In this guide, we’ll explore how to modernize old methods of insurance verification that cost practices millions and build an automated workflow that protects your bottom line.
Table of Contents:
- Insurance Eligibility Verification FAQs
- Insurance Eligibility Verification: Legacy vs Modern Processes
- Common Medical Insurance Eligibility Verification Pitfalls
- Best Practices for Effective Insurance Eligibility Verification
- What to Look for in Insurance Verification Software
Insurance Eligibility Verification FAQs
What is health insurance eligibility verification?
Health insurance eligibility verification is the process of confirming a patient's insurance coverage status with the payer prior to a medical appointment. However, true verification goes beyond a simple "Active" or "Inactive" check. It involves validating the specific benefits associated with the patient's plan, including copayments, coinsurance, deductibles, and coverage limits for specific services.
Why is insurance eligibility verification important?
The impact of verification ripples through every department of your organization. Optimizing this process provides the following benefits:
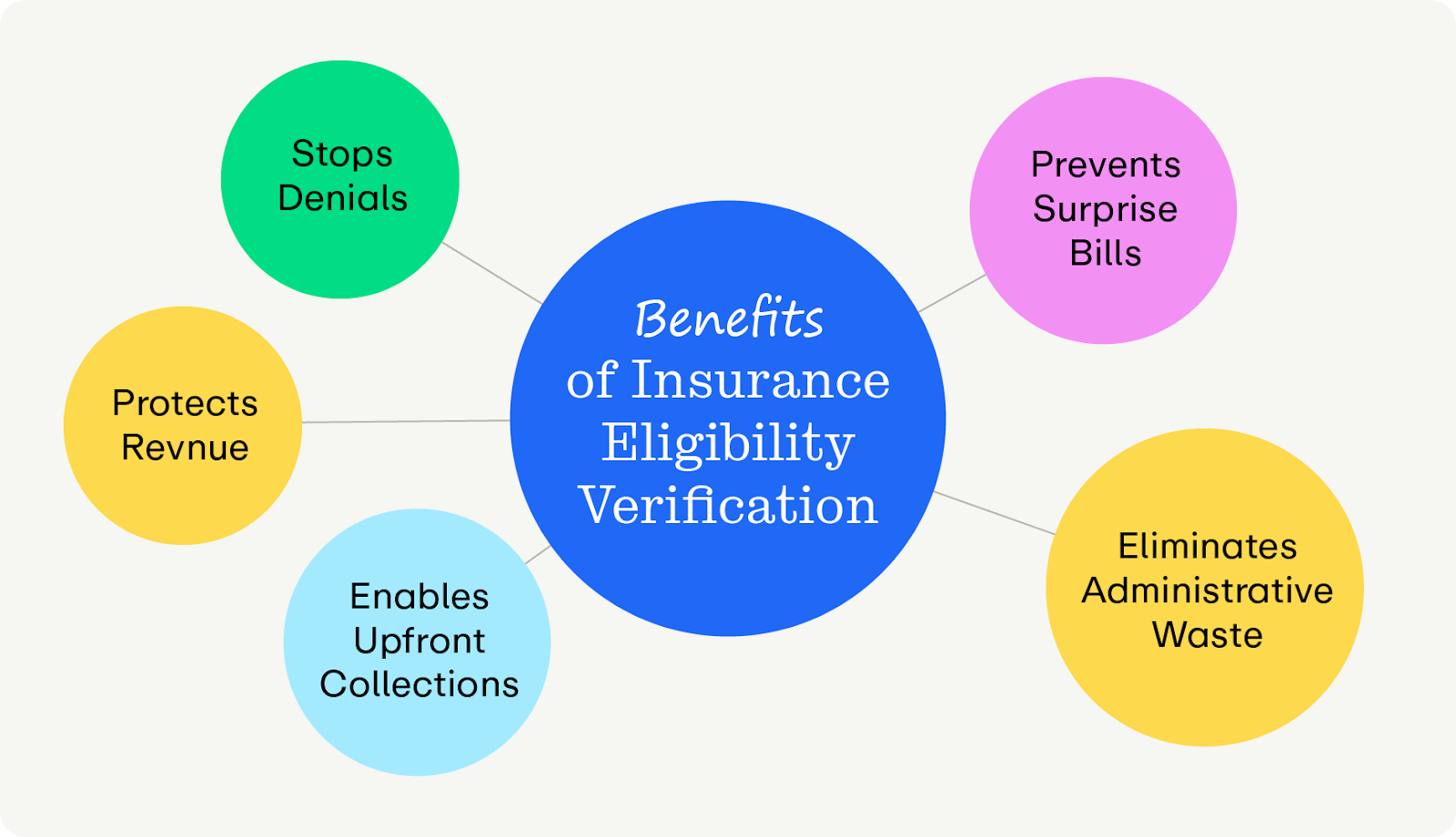
- Stops the #1 cause of denials. Studies show that nearly a quarter of denials are eligibility-related. Stopping these at the front door is the single most effective way to clean up your claims process.
- Protects revenue integrity: Insurance verification ensures you are paid the "allowable" amount you contracted for. Without it, you can’t reliably predict revenue.
- Enables upfront collections: Accurate verification empowers your staff to collect the patient's financial responsibility before rendering the service, which greatly increases collection rates.
- Prevents surprise bills. Surprise bills harm patient satisfaction and can turn them away from your practice. By verifying benefits upfront, you can give them a clear cost estimate, improving satisfaction and trust.
- Eliminates administrative waste. Reworking a denied claim once costs an average of $25 in labor, and many claims go through the process multiple times. Preventing that denial costs pennies in automation software.
What is the difference between "eligibility" and "benefits"?
While the terms are often used interchangeably, they represent two distinct layers of insurance verification:
- Eligibility determines if the patient is a recognized member of the insurance plan. It validates these foundational data points:
- Is the policy currently active?
- Do the Name, Date of Birth, and Member ID match the payer’s records exactly?
- What are the effective start and end dates of the coverage?
- Benefits determine the financial specifics of the patient's coverage relative to the services you provide. It validates the following aspects:
- Does the plan cover the specific CPT codes scheduled (e.g., is "Physical Therapy" a covered benefit)?
- What is the specific copay, coinsurance percentage, and remaining deductible for this service type?
- Are there caps on the number of visits or requirements for prior authorization?
Essentially, being "Active" does not mean "Covered." A patient can have an active policy that explicitly excludes the specific procedure you perform. If your verification process stops at eligibility, you remain at high risk for denials based on benefit exclusions.
When should insurance eligibility verification happen?
Patient coverage frequently changes between visits, often influenced by job changes or other shifting economic circumstances. To fully protect your revenue, continuously monitor their insurance coverage with a cadence like this:
- Upon booking: Run an automated check the moment the patient books an appointment. This flags major issues weeks in advance, giving you time to contact the patient to update their info without rushing.
- 48–72 hours prior: Run a batch check for all upcoming appointments in the next week. This confirms that benefits are still valid and allows you to generate a precise financial estimate to send to the patient before they arrive.
- Morning of appointment: Run a final spot check for high-value procedures, just in case something might have changed.
The only way to check insurance efficiently and frequently is by using a software that offers Real-Time Eligibility (RTE) checks, like Promptly. We’ll explore more of Promptly’s features later.
Insurance Eligibility Verification: Legacy vs Modern Processes
Manually checking on insurance is very time-consuming and cumbersome for your team. Take a look at how smart eligibility verification processes differ:
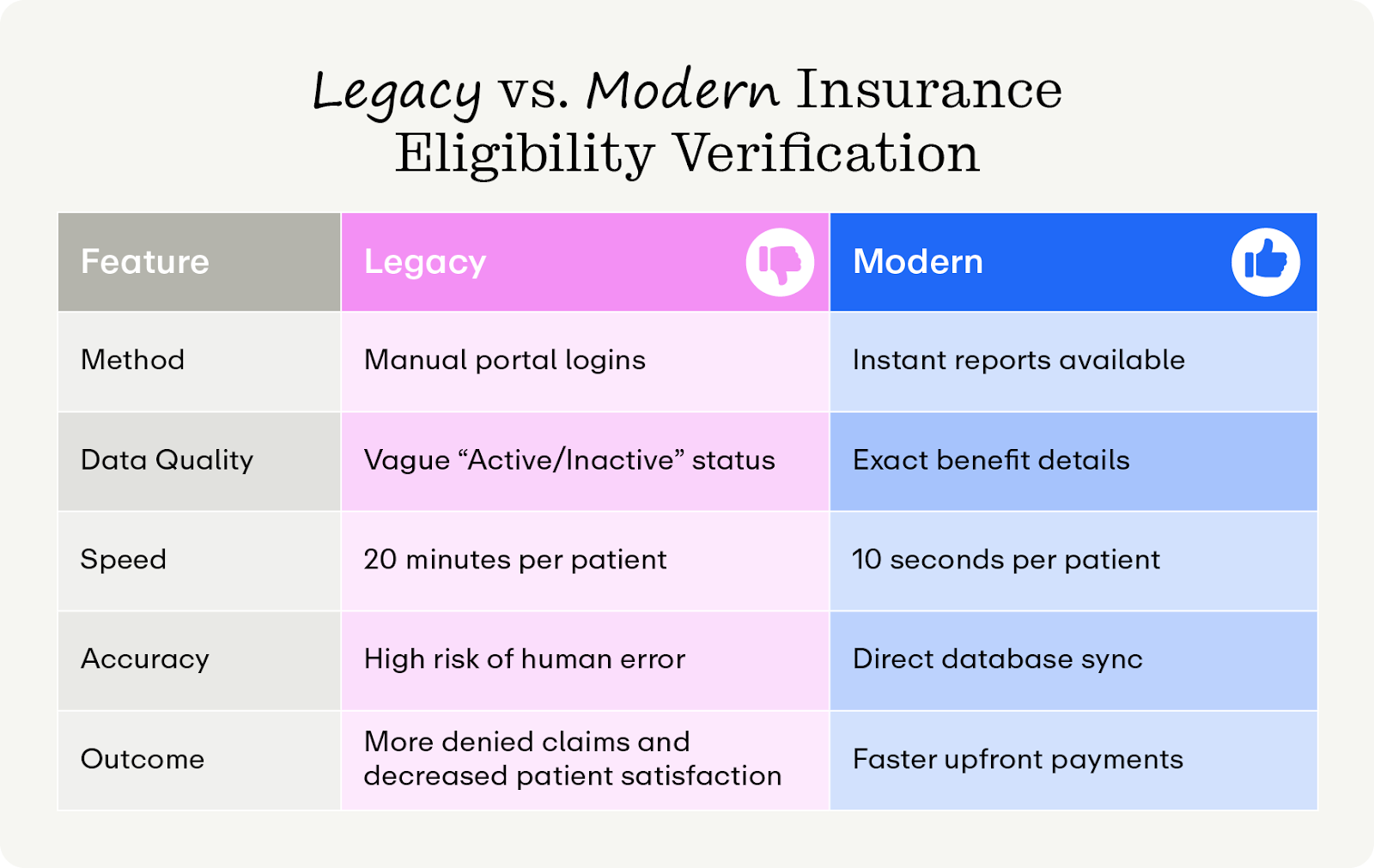
- Method: Instead of spending hours on hold or logging into different websites to copy-paste data, the modern system runs automatically in the background, or on demand if needed—allowing staff to read the report without ever leaving the PM system.
- Data quality: While legacy methods often return a binary "Active/Inactive" status, modern RTE provides a granular breakdown of benefits, including accumulators, co-insurance percentages, and specific service caps directly from the payer.
- Speed: Manual checks take approximately 15–20 minutes per patient, whereas RTE checks take roughly 10 seconds per patient (or can process hundreds of patients overnight in a batch).
- Accuracy: Automation eliminates the typos and ID transpositions common with manual entry, ensuring total data integrity by pulling information directly from the payer’s database.
- Outcome: Shifting from manual to automated verification replaces staff burnout and awkward financial surprises with clean claims, confident upfront collections, and happier patients.
Common Medical Insurance Eligibility Verification Pitfalls
Even practices that think they are verifying insurance often fall into specific traps. These are the nuances that generic software or inexperienced staff will miss, leading to preventable denials:
- Confusing "active" with "covered": As previously mentioned, a patient may have an active policy, but their plan might have a "waiting period" for pre-existing conditions or exclude specific elective procedures entirely. If you don't check the benefit details, you risk a denial for "Benefit Maximum Reached" or "Service Not Covered."
- Coordination of Benefits (COB) errors: This occurs when a patient has two insurance plans (e.g., a commercial plan and Medicare, or a child covered by both parents). Failing to identify which payer is primary and which is secondary is a guaranteed denial.
- Ignoring service-specific deductibles: Many modern plans have "tiered" benefits. For example, a patient might have a $500 deductible for general care but a separate $2,000 deductible for specialized care. Quoting the wrong deductible leads to lost revenue and patient trust.
- Data entry errors: Entering incorrect identification data, transposing Member ID numbers, or missing a middle initial can prevent the claim from matching the payer’s records.
Best Practices for Effective Insurance Eligibility Verification
The cornerstone of an effective verification process is a proactive approach. Instead of a "reactive" model (fixing denials when they occur), implement efforts to prevent denials before they happen. Here’s the blueprint for a world-class verification workflow:
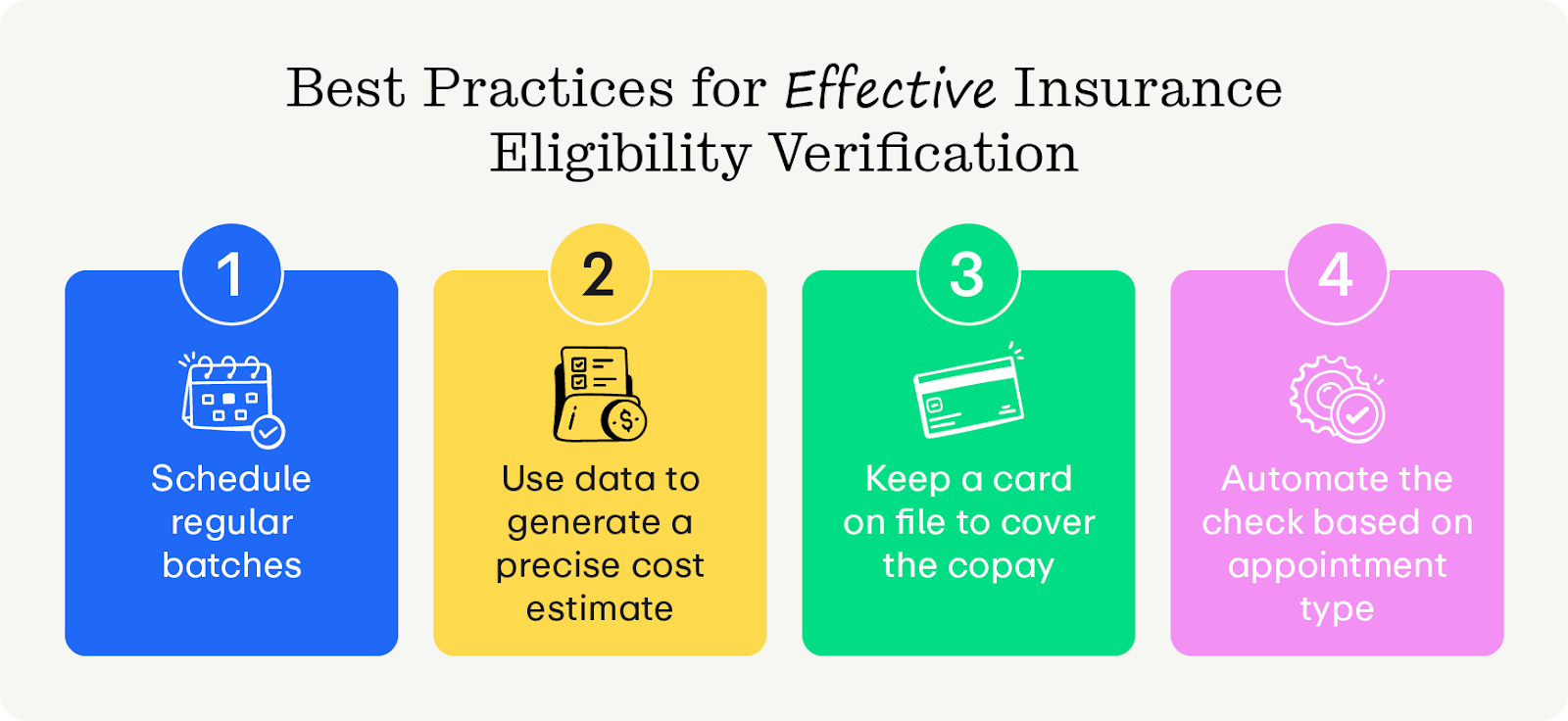
- Run batch checks overnight: Stop checking patients one by one as they walk in. Configure your software to run the entire schedule for the next 3 days automatically every night. When your staff arrives, they should manage by exception—only looking at the "Red Flags," not the patients who cleared successfully.
- Generate Precise Cost Estimates (PCE): Patients today are consumers who want to know the price tag. Use your eligibility data to calculate the exact patient responsibility (which is usually the cost of your services minus deductible and copay) and present this to the patient via text or email before the visit.
- Verify and secure payment upfront: Don't just verify coverage; verify the ability to pay. Once benefits are confirmed, keep a credit card on file to cover the estimated copay. This secures your revenue after the appointment.
- Automate triggers based on appointment type: Not all appointments need the same level of scrutiny. Set up rules to trigger deep verification immediately for different segments of patients (e.g., new patients or those requiring certain procedures) while running lighter checks for routine follow-ups.
Accidents and mistakes happen all the time in medical billing. Taking these small steps ensures you can put your best foot forward and collect the most money possible, as quickly as possible.
What to Look for in Insurance Verification Software
To truly automate your revenue cycle, you need a robust solution with features like:
- RTE checks: The ability to check status instantly is crucial for walk-in clinics or last-minute schedule add-ons.
- Batch processing: Your software must be able to ingest your entire schedule and process hundreds of checks simultaneously without crashing, allowing you to complete critical tasks with peace of mind.
- Deep PM software integration: The software should read the benefits from the payer and automatically transfer them with the correct fields in your PM system, eliminating manual data entry entirely.
- PCE calculation: Look for a tool with a built-in algorithm and calculator that applies your specific fee schedule to the patient’s benefits to determine a clear dollar amount.
- Coverage for all payers: Prioritize connectivity to a wide range of commercial and government payers (including Medicare/Medicaid) to ensure you aren't forced back to manual insurance processes for niche plans.
What’s the best health insurance eligibility verification software?
When you evaluate the landscape based on connectivity, automation, and financial integration, Promptly emerges as the superior choice for modern practices. Unlike other solutions, Promptly is built with a unique architecture that seamlessly merges clinical intake with financial clearance. Take a look at some of our key features:
- Specialty-specific verification logic: Generic tools often fail complex specialties. For example, Promptly handles split-benefit verification for eye care, verifying both medical and vision policies simultaneously and applying logic to determine which covers the specific visit.
- Automated cost transparency: Promptly integrates eligibility data with your fee schedules to provide accurate, automated patient cost estimates.
- Seamless integration: Promptly connects directly with major PM systems to update insurance details without staff intervention. We push the verified data back into your system and flag the chart if coverage is invalid.
- Unlimited RTE checks: You shouldn’t have to pick and choose when you need a RTE check. With Promptly, you can leget the information that you need, whenever you need it, ensuring accurate numbers and happy patients.
Not convinced yet? Our stats don’t lie. Practices that switch to Promptly’s automated insurance verification engine see:
- 60% decrease in staff time spent on phone/portals.
- 48% gap closure in verified insurance compared to competitors like Clearwave.
- $88,000 average annual savings by consolidating intake, verification, and payment vendors into a single platform.
Moreover, Promptly is a holistic patient engagement platform, meaning you can manage your practice’s reputation, schedule appointments, conduct intake, manage referrals, and communicate with patients all in one place. It’s the best solution for practices that want to power their practices with a user-friendly platform built for patient satisfaction.
Wrapping Up
The days of crossing your fingers and hoping a claim gets paid are over. In a healthcare environment with shrinking reimbursements and rising costs, you cannot afford to leak 24% of your revenue to preventable eligibility errors. Don't let easily-avoidable errors take another dollar from your practice!
To set your practice up for success, start by quantifying the exact cost of your current manual process. Ask your billing manager to identify the total dollar value of eligibility-based denials from the last quarter and add the estimated labor cost of staff time spent on payer portals. Bringing this concrete number to your next partnership meeting shifts the conversation from buying software to plugging a verified revenue leak, making the decision to modernize increasingly valuable.
Want to learn more? Check out our other helpful healthcare management resources:
- Digital Patient Intake Guide for 2025: Key Insights for Healthcare Practices. Patient intake is an essential part of insurance eligibility verification. Use this guide to understand where you stand.
- 7 Workflow Automation Strategies To Save 1,700+ Staff Hours Annually. You read that right! We’ve cracked the code of saving time and money with smart workflows, and you can get started with this guide.
- Why Specialty Practices Need Integrated Digital Solutions Beyond Patient Portals. Digital portals can be unwieldy and bog down the patient experience. Understand the importance of digital solutions in cultivating positive patient experiences here.
Stop guessing and start collecting.
Get a demo of Promptly’s Real-Time Eligibility tool today.
Related Posts
About the author
Dr. Anish Kapur is a physician and tech entrepreneur advancing healthcare through innovation. He co-founded one of the first cloud-based EMR systems for specialists and now leads Promptly Technology Inc., whose Patient Experience Suite™️ helps specialty practices streamline workflows, boost patient engagement, and accelerate revenue—all in one modern platform.

Share this article:






